On June 24, Laura Schneider, the senior clinical director at AMSURG, explained some key issues and tips for running drills in ambulatory surgery centers. With over 40 years of experience in the healthcare industry, Schneider has dealt with most situations for which these drills are built to help staff be ready.
One of the biggest differences between hospitals and surgery centers is the amount of resources they have, so when ASCs are preparing for potential emergencies, it’s important that they allocate their resources and staff effectively. “There’s not always extra people around, so you’ve got to use your resources wisely,” Schneider said. “You want to make sure you’re prepared.”
“Everyone should do a hazard vulnerability assessment at their center,” Schneider added. These assessments are for all kinds of possible disasters. They look at four things: the likelihood of a disaster happening, risk associated, mitigation and preparedness. This allows a facility to figure out how prepared it is for disasters and where the gaps are.
Texas ASC Fire Prevention
The first type of drill Schneider went over was fire drills. There are five major requirements when it comes to fires, and Schneider covered each step in detail.
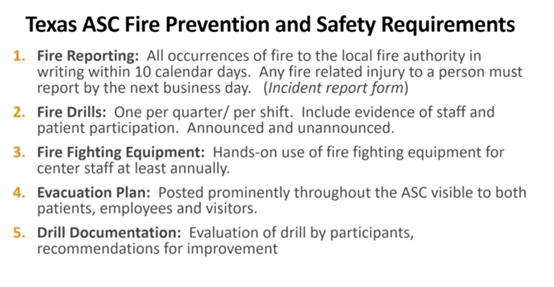
Since each drill requires documentation, Schneider recommended using sign-in sheets to document all staff in attendance and to be sure to include an evaluation that asks questions about what worked and what didn’t, as well as what each member learned during the drill. This feedback will be helpful to adapting the drill to suit your facility best.
Medical Building Evacuation
There are several reasons for evacuations at ASCs—drills, bomb threats, gas leaks—and with all the moving parts that go into a facility, there are several aspects to think about when it comes to evacuating the building. The first thing to do is stay calm and start the process.
When it comes to patients, it’s important to figure out the most efficient way to get them evacuated. Some facilities are two stories, and not every patient will be able to walk. For these situations, Schneider recommended a flexible stretcher to get them downstairs. If possible, she also suggested securing patient valuables and having employees do the same. Sometimes, once evacuated, there’s no going back in. If you have the capacity to grab your cell phone and car keys, you should do so, just in case. It’s also critical to have an evacuation kit of some sort filled with medical supplies, such as a blood pressure cuff and IV tape so that you can continue to provide care for patients if you are stuck outside the building for long periods of time.
Code Blue
While visiting one of her facilities, Schneider helped with an actual code blue that occurred at the ASC. She thought the safest thing she could do was man the crash cart and found that the abundance of labels on the crash cart was overwhelming for the high-stakes situation. Therefore, it switched to bigger, all-encompassing labels instead.

The following week, the center staff and providers had a staff meeting to evaluate the drill. Some concerns that came up during debriefing were that no one was sure what their role was, and it led to some confusion and some important steps being skipped over or ignored. To solve this issue in future drills and be prepared for the real thing, one center came up with role cards so everyone knows what to do during the drill; they switch up which staff members get what card so everyone is familiar with each main position in a code blue drill.
One other pro tip Schneider offered was to make sure staff knows what a code blue alarm sounds like in each part of the facility. She told a story about being in a center leader’s office once when a code alarm was going off and how the lead was uncertain what the sound was. Finally, the lead said she thought it was their code blue alarm. “So that’s a very important lesson: See what your code alarm sounds like in different parts of the building so you’re familiar with it,” Schneider said.
Incapacitated Provider
Often, staff members don’t know about their coworkers’ medical conditions and staff are not supposed to treat other coworkers or physicians because they aren’t patients at the center. Doing so could lead to causing more harm or a possible malpractice suit. If it’s life or death, that is OK to treat the person with life saving measures. Otherwise, staff should wait for emergency medical services to arrive.
Active Shooter/Dangerous Intruder
In the case of active shooters, the three critical steps are to run, hide and fight, if necessary. Everyone has to be trained to follow those three steps because in situations like this, there is no time to go around and make sure everyone is okay or know what to do. “It’s another situation where literally everyone is on their own, and they have to have that training to know what to do,” Schneider said.
Bomb Threat
When it comes to bomb threats, every threat should be treated seriously until proven otherwise, and proper procedure should be followed. If your facility doesn’t have a panic button, Schneider recommended getting one. These will alert the police that something is wrong at your ASC so they can call or come investigate the situation.
Oftentimes, bomb threats are called in. Schneider ran a drill at one of her facilities and called pretending to be someone who planted a bomb in the facility. During the drill, she found that the staff member on the other line was not attempting any empathy with her and, instead, going directly down the list of questions for this scenario. From this experience, Schneider suggested attempting to address the hostile person’s concerns or having some empathy for whatever frustrations led them to make the bomb threat in the first place. “Keep in mind you want to try and feel what they’re feeling and talk them out of it,” she said. She also highlighted the significant amount of bombings that occurred over the years to emphasize the likelihood of a potential bomb threat.
Hazardous Spill
Hazardous spills occur more often at facilities that use high-level disinfectant, such as endoscopy centers, but it’s important for every type of center to be prepared for this potential hazard. These disinfectants are extremely irritating to the skin and eyes when people try to clean them up without proper safety measures. Every facility should have a hazardous spill safety kit. Before attempting to clean up a spill of a toxic solution, neutralizer should be poured over the spill and left for 15 minutes to neutralize the solution so it’s safe to clean up.
In all situations, the key is to stay calm and be prepared. “Have the drills, and have everyone talk about it,” Schneider said. By continuing to practice, prepare and adapt the drill based on the feedback provided, ASCs will be one step closer to being able to handle anything that comes their way.

