Clinical Specialist Talks How to Combat Hazardous Surgical Smoke in the OR
In August, Catherine Kane, clinical specialist at Pall Corporation, spoke to TASCS members about the dangers of surgical smoke in the operating room and how to deal with this hazard in surgery centers.
“Each year, an estimated 500,000 workers, including surgeons, nurses, anesthesiologists and surgical technologists, are exposed to laser or electrosurgical smoke,” Kane said, citing OSHA.
Surgical smoke comes from the smoke in laser and electrosurgical units (ESU) and in the form of a mist through ultrasonics. It is a hazardous plume that is 95% water vapor and 5% other particles, some of which remain in the air for up to 20 minutes and penetrate the deepest part of the lungs. This smoke becomes evenly distributed throughout the OR, traveling at up to 40 mph, so everyone is equally affected.
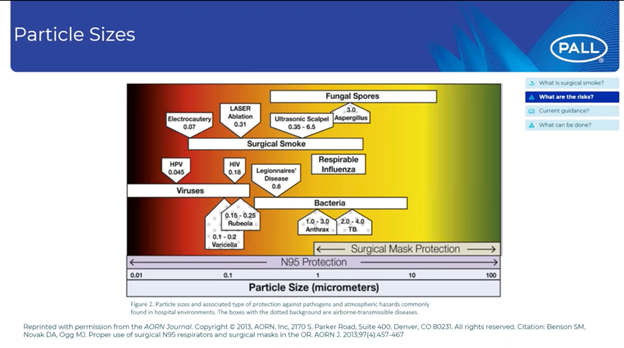
A regular surgical mask can only protect you from so much, Kane pointed out, so unless you are using an N95 mask in the OR, there are several particles to which you and your team could be vulnerable.
Beyond the dangers of transmission, though, the smoke also has the potential of reducing visibility during laparoscopic surgery, which could lead to temporary lack of control in the OR.
For patients and staff alike, the exposure to harmful chemicals like carbon monoxide and benzene are common from surgical smoke, and noxious odors may lead to headaches or irritation of the eyes, nose and throat.
To further contextualize the dangers, Kane referenced a 1981 study that showed lasering one gram of tissue was equivalent to smoking three cigarettes, while electro-cauterizing one gram of tissue was equal to smoking six cigarettes. In a more recent 2012 study, the daily average of surgical plume produced was shown to be equal to 27-30 cigarettes.
After educating the TASCS members on the dangers of surgical smoke, Kane spoke on the solutions and federal guidelines in place for creating a safe OR in hospitals and ambulatory surgery centers. One of the most important aspects is using a filtering device or closed evacuation system.
The Association of periOperative Registered Nurses recommends to also take special care for COVID-19 patients. The use of energy-generating devices during surgical procedures may be considered aerosol-generating procedures, which are known to present higher risk to OR staff in presence of COVID-19. “In order to protect your staff, you just have to assume it could potentially be in your surgical smoke,” Kane said.
The International Federation of Perioperative Nurses and the Centers for Disease Control and Prevention also emphasize recognizing surgical smoke as a hazard and using proper ventilation and smoke evacuation methods.
With all this in mind, the first line of defense should be to adopt an evacuation program and then educate staff and wear appropriate PPE in the OR.
Kane referenced the Pall Corporation’s laparoscopic smoke filter as an example of a quality filter to look for, due to its validated efficiency, viral claims and ULPA rating. Even at its weakest point, the filter has a 99.9% retention rate for inorganic material, viruses, liquids and other harmful particles.


