Infection preventionist and medication safety experts spoke with TASCS members about the dangers of negligent injection practices and tips for safe injection practices.
Safe injection practices are a significant part of keeping patients safe, as they help prevent the spread of diseases, miscommunication in drug doses and the contamination of medications. “The primary objective in injection safety is preventing transmission of Hepatitis B, Hepatitis C and human immunodeficiency viruses,” Maggie Miller, an infection preventionist with ECRI, told Texas Ambulatory Surgery Center Society (TASCS) members during a recent virtual town hall. She also spoke to the more general significance and procedural standards for injection safety.
In 1985, the Centers for Disease Control and Prevention created universal precautions that laid the groundwork for these standards to continue to evolve over the years. The CDC later partnered with the Safe Injection Practices Coalition to create the One and Only Campaign, a public health effort to eliminate unsafe injection practices.
In order to manifest safe injection practices, management should ensure they have enough supplies so staff aren’t tempted to re-use syringes and buy the smallest dosage possible that will work effectively. Providers should never administer medication from the same syringe for more than one patient. They should also practice proper hand hygiene and limit their use of multi-dose vials. Providers should dispose of needles as soon as possible after use in a puncture-resistant receptacle that is easily accessible and that has a biohazardous label.
Christina Michalek, medication safety specialist with the Institute For Safe Medication Practices (ISMP), talked with TASCS members about the significance of safe injection practices in surgery centers specifically.
Michalek identified several sterile compounding risks that could lead to potential harm, including the reuse of medication vials meant for single use, compounding outside of environmental controls and preparing medications in commercially available syringes of .9% sodium chloride that are not meant for medications.
One of the most common errors reported are those involving labeling issues. Michalek shared a story of a 15-year-old boy who had a history of malignant hypothermia and received an unlabeled syringe. The surgeon thought the syringe contained bupivacaine, but it actually contained epinephrine. When the patient’s heart rate started to increase, the surgeon initially thought it had to do with the malignant hypothermia, and it wasn’t until the patient developed ventricular tachycardia that they realized it was a medication error. Fortunately, the patient recovered, although he had to be transferred to a higher level of care.
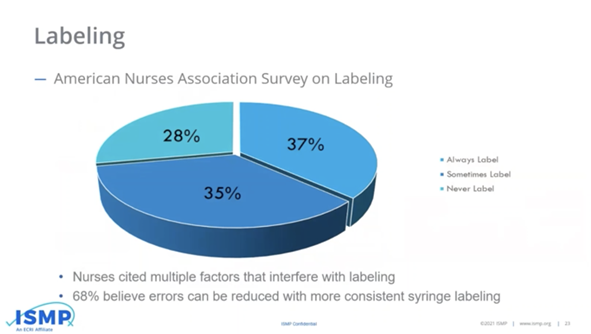
A decade-old survey from ISMP showed only 37% of nurses always label their syringes. In 2018, ISMP checked in again about labeling syringes, and there has not been much improvement; only about half of nurses reported they always label syringes that are prepared away from the patient’s bedside.
For best practices in surgery centers, Michalek listed several things you can do.
- Purchase commercially prepared, premixed products whenever possible
- Don’t dilute push IV medication
- Don’t use commercially available flush syringes or cartridge-type syringes
- Label all prepared syringes
- Never pre-label syringes in anticipation of their use
- Monitor compounding
- Provide training for staff on these best practices
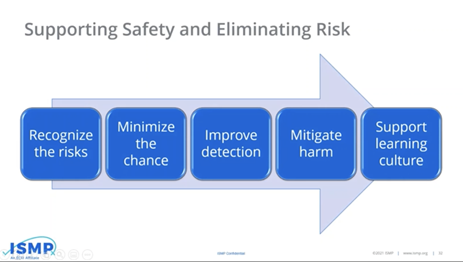
Overall, it’s important to support the safety of patients and eliminate the risks to the best of our ability, Michalek said. She added that ISMP’s website provides safety guidelines for adult IV push medications, as well as several other resources to help guide the best injection practices at ASCs and beyond.

